Improving treatment for disease of this essential organ
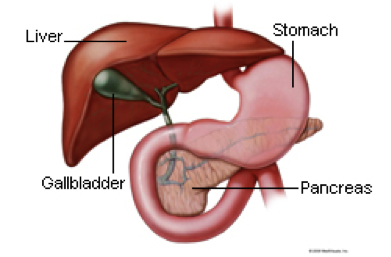
The pancreas is a critical organ due to its role in digestive and endocrine function. Surgery for pancreatic conditions addresses either tumors of the pancreas or conditions that cause inflammation (pancreatitis).
Pancreatitis may be either acute or chronic. In either case, the medical team can often manage the patient’s condition medically (without invasive intervention). However, compromised pancreatic tissue can atrophy or become infected. If the condition is severe or longstanding and resists conservative therapy, surgery may be necessary.
Pancreatic tumors are uncommon but may be either malignant or benign. Malignant tumors in this organ, however, bring with them such a serious prognosis that they are one of the leading causes of cancer death. Pancreatic cancer can sometimes be treated through surgery. For more on surgical treatment of pancreatic tumors, see Aria’s Division of Surgical Oncology.
Surgery of the pancreas most often involves removing the diseased portion of the organ. These surgical procedures are major operations, requiring several hours in the operating room. Patients remain in the hospital for about a week after the surgery and will need several weeks to more fully recuperate. Other surgical procedures for pancreatitis include fluid drainage from the pancreas or surgical opening of the pancreatic duct.
In some cases, the surgical team can perform pancreatic surgery laparoscopically. This makes the duration of surgery and recovery shorter.
The pancreas is surrounded by a lattice of nerves and by other essential organs, and is therefore sensitive from a pain-management perspective. Skilled use of pain control is essential for patients suffering from pancreatic conditions or recovering from surgery.
Some patients will require repeat operations to remove all of the diseased areas of tissue resulting form severe pancreatitis. In addition, many patients develop diabetes if they have lost a significant portion of their pancreas to pancreatitis or pancreatic surgery. This may partly or largely resolve, given time.
 ERCP is a procedure that enables your physician to examine the pancreatic and bile ducts. A bendable, lighted tube (endoscope) about the thickness of your index finger is placed through your mouth and into your stomach and first part of the small intestine (duodenum). In the duodenum a small opening is identified (ampulla) and a small plastic tube (cannula) is passed through the endoscope and into this opening. Dye (contrast material) is injected and X-rays are taken to study the ducts of the pancreas and liver.
ERCP is a procedure that enables your physician to examine the pancreatic and bile ducts. A bendable, lighted tube (endoscope) about the thickness of your index finger is placed through your mouth and into your stomach and first part of the small intestine (duodenum). In the duodenum a small opening is identified (ampulla) and a small plastic tube (cannula) is passed through the endoscope and into this opening. Dye (contrast material) is injected and X-rays are taken to study the ducts of the pancreas and liver.